
ACNÉ AND STEROIDS

1. INTRODUCTION
Acne is one of the most telltale side effects of steroid use, and it is also highly unappealing. For this reason, any steroid user aims to minimize it or, if possible, eliminate it entirely to achieve clear and healthy-looking skin.
The reasons for acne appearance are diverse and usually result from a combination of genetic, environmental, hormonal, and bacterial factors. Among these, the use of anabolic steroids also plays a significant role.
2. CAUSES OF ACNE
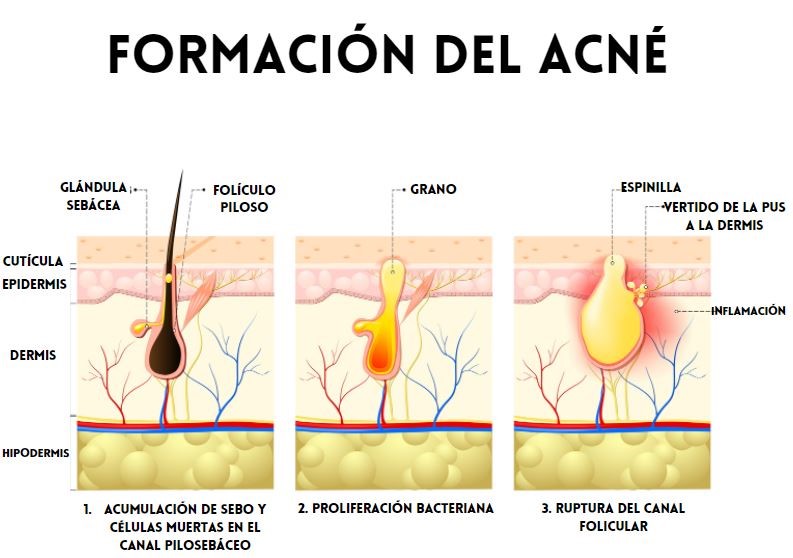
- Excessive Sebum Production: Acne is often associated with excessive sebum (oil) production by the skin’s sebaceous glands.
This issue worsens with inflammation and an altered lipid profile, particularly an increase in total cholesterol and LDL levels.
Excess sebum can clog skin pores, fostering bacterial growth and leading to the formation of pimples and blackheads.
- Hormonal Changes: Hormonal fluctuations, such as those occurring during puberty, pregnancy, or the menstrual cycle, can trigger excessive sebum production and increase the risk of acne.
Androgens, such as testosterone, stimulate sebaceous glands and contribute to acne development.
Drastic hormonal changes can significantly worsen acne.
- Bacterial Proliferation: The bacterium Propionibacterium acnes (P. acnes), commonly found on the skin, can proliferate under conditions of excess sebum and clogged pores.
Staphylococcus aureus also plays a role, with both bacteria being major contributors to acne vulgaris.
This bacterial overgrowth can lead to inflammation and the formation of inflamed pimples.
Additionally, these bacteria proliferate more easily in cases of estradiol deficiency, which is often seen with indiscriminate use of aromatase inhibitors rather than proper cycle management.
- Genetic Factors: Genetic predisposition can also influence acne susceptibility. Those with a family history of acne are more likely to develop the condition.
- Environmental Factors: Using comedogenic skincare products (which clog pores), exposure to polluted environments, or excessive friction on the skin can all contribute to acne development.
- Stress: While stress does not directly cause acne, it can worsen existing acne by increasing stress hormone production, such as cortisol, which influences sebum production and triggers breakouts.
3. HOW ANABOLIC STEROIDS AFFECT ACNE
The skin contains androgen receptors, which explains why conditions like acne vulgaris and folliculitis are observed in 43% of anabolic steroid users.
Skin biopsies in this population reveal:
Hypertrophy of sebaceous glands.
Increased skin surface lipids.
Elevated populations of skin bacteria such as P. acnes and S. aureus.
The clinical presentation can vary, ranging from initial onset of acne or worsening of pre-existing acne to the development of severe forms like acne conglobata or acne fulminans.
Severe Types of Acne Associated with Steroid Use
ACNE CONGLOBATA:

- Description: A severe form of nodulocystic acne that primarily affects young men, although it can also occur in women.
Characteristics:
- Deep, painful lesions: Large nodules and cysts form beneath the skin, often causing significant discomfort.
- Abscess and fistula formation: Nodules and cysts may ooze pus, forming abscesses (collections of pus) and fistulas (connections between deep skin lesions).
- Severe scarring: Due to the intense inflammation and cyst rupture, acne conglobata usually leaves significant scars.
Distribution: It affects large areas of the body, including the face, chest, back, and buttocks.
Causes and Triggers:
- Hormonal imbalances: Although not completely understood, hormonal disruptions may trigger this condition. It is sometimes associated with polycystic ovary syndrome (PCOS) in women.
- Genetic factors: There may be a genetic predisposition, especially if there is a family history of severe acne.
- Anabolic steroid or testosterone use: These substances can trigger or worsen acne conglobata.
ACNE FULMINANS:
Description: A rare and severe form of acne that appears suddenly, primarily in adolescent males. It is considered a dermatological emergency due to its rapid onset and associated systemic symptoms.

Characteristics:
Severe skin lesions: Sudden development of inflamed nodules and ulcers, often extremely painful. These lesions may ooze pus and form crusts.
Systemic symptoms:
Fever.
Muscle and joint pain (especially in shoulders and knees).
Fatigue.
Weight loss.
Increased levels of inflammation detectable in blood tests.
Causes:
- Severe hormonal imbalance: Believed to be related to an abrupt increase in hormones, causing massive sebum production and sebaceous gland inflammation.
- Genetic predisposition: This may also play a role.
- Anabolic steroid use: Similar to acne conglobata, anabolic steroid use can trigger acne fulminans.
- High-dose isotretinoin treatment: In rare cases, a severe reaction to isotretinoin (a common acne treatment) can trigger this condition.
SUMMARY OF MAIN ACNE CAUSES
- Sebum overproduction by sebaceous glands.
- Follicular colonization by Propionibacterium acnes.
- Abnormal keratinization processes.
- Release of inflammatory mediators in the skin.
ADDITIONAL FACTORS
Dietary Factors: Saturated fats, trans fats, and a worsened lipid profile contribute to acne by creating an environment conducive to excess sebum production.
Excessive consumption of animal products, especially red meats and fats, due to their methionine and dietary cholesterol content, can worsen acne, particularly when abused.

Follicular Hyperkeratinization: This term refers to abnormal behavior of skin cells within hair follicles. Skin cells (keratinocytes) become cohesive and shed rapidly, clogging follicular openings.
Inflammation appears to trigger these processes, with hyperkeratinization following as a secondary step. As mentioned earlier, inflammation can result from increased sebum production.
Additionally, P. acnes thrives in sebum-rich environments, further exacerbating inflammation.
WHICH INFLUENCE HAS STEROIDS?
The use of high doses of steroids, as often seen in bodybuilding, increases androgen levels in the body.
These androgens, particularly testosterone and dihydrotestosterone (DHT), stimulate the skin’s sebaceous glands to produce more sebum (oil).
Excessive sebum clogs pores and hair follicles, promoting the proliferation of bacteria like Propionibacterium acnes, which leads to inflammation and the formation of pimples, pustules, and cysts.
The skin contains androgen receptors, making it highly sensitive to hormonal changes. Anabolic steroids directly stimulate these receptors, increasing sebaceous gland activity.
Specific Effects:
Elevated testosterone levels are converted into DHT, which is more androgenic than testosterone itself.
DHT is particularly effective at increasing sebum production, exacerbating skin issues, contrary to the belief that estradiol was the main culprit.
This process affects areas with more sebaceous glands, such as the face, back, and chest, leading to increased acne in these regions.
Androgens also increase inflammation in the body, which further promotes acne formation. Additionally, an imbalance in therapy or indiscriminate use of aromatase inhibitors can lower estradiol levels, worsening acne or triggering its onset.
Markers to Consider:
Inflammatory markers such as high-sensitivity C-reactive protein and homocysteine are relevant indicators of systemic inflammation contributing to acne.
Key Actions to Manage Acne:
Conduct intra-cycle blood tests to monitor estradiol levels.
If estradiol is low, address it by reducing DHT derivatives and/or increasing testosterone levels.
When hormonal adjustments are insufficient, consider additional treatments, ranging from topical applications to more aggressive systemic options.
Contrary to previous beliefs, estradiol is not the cause of acne. Instead, excessive androgens and overly androgenic pharmacological therapies predispose individuals to acne due to estradiol deficiency.
4. WHAT TREATMENTS ARE AVAILABLE?
Acne treatments vary widely. Some target sebum production, while others act as antibiotics, and often both. Treatment plans often combine approaches, tailored to the severity of the acne and using an appropriate protocol.
Topical Treatments:
Though safer and effective, they can be tedious to apply, especially over large areas like the back.
They must be applied not only to active acne lesions but also to the entire area to prevent new breakouts.
Oral Treatments:
These are often more practical for severe or widespread acne.
4.1. BENZOYL PEROXIDE
Benzoyl Peroxide is an organic compound widely used as a topical treatment for acne. It is considered one of the most effective and commonly prescribed treatments for this skin condition due to its ability to target multiple underlying causes of acne.

Below is a detailed explanation of how it works and its benefits:
MECHANISM OF ACTION
Benzoyl peroxide is effective in reducing the amount of bacteria on the skin, particularly Propionibacterium acnes (P. acnes), which is one of the main culprits of inflammatory acne. This bacterium colonizes blocked pores and contributes to the formation of pimples and pustules.
Benzoyl peroxide releases oxygen into the skin, creating a hostile environment for anaerobic bacteria (like P. acnes), which cannot survive in the presence of oxygen.
Benzoyl peroxide helps exfoliate the top layer of the skin by removing dead cells that can clog pores. This keratolytic action promotes cell renewal, preventing the formation of comedones (blackheads and whiteheads).
Although its main action is not directed at controlling sebum, benzoyl peroxide also has a mild effect on reducing oil production in the skin, which helps control the formation of blocked pores.
Anti-inflammatory properties: By reducing bacteria in the pores and decreasing inflammation, benzoyl peroxide also helps soothe the redness and swelling of acne lesions.
Benzoyl peroxide not only treats existing lesions but also helps prevent the formation of new ones by unclogging pores and reducing the amount of bacteria.
It is often combined with other topical or systemic treatments to improve efficacy. For example, it can be combined with topical antibiotics (like clindamycin) or retinoids (like adapalene) to address acne from multiple angles.
Benzoyl peroxide is available in different concentrations, typically ranging from 2.5% to 10%, in gels, creams, and facial cleansers.
Lower concentrations are usually as effective as higher ones but with less risk of irritation.
4.2-TEA TREE OIL:
Tea tree oil is an essential oil extracted from the leaves of the Melaleuca alternifolia tree, native to Australia. This oil has been used for centuries due to its antimicrobial, antifungal, and anti-inflammatory properties, making it a popular remedy for treating skin infections, irritations, and acne.

MECHANISM OF ACTION
- Antimicrobial: The oil contains compounds such as terpinen-4-ol, which have the ability to eliminate bacteria and prevent skin infections.
- Anti-inflammatory: Reduces inflammation and redness associated with acne breakouts.
- Antiseptic: Helps cleanse pores and prevent secondary infections.
- Sebum Regulation: Helps balance sebum production, reducing shine and clogged pores.
Tea tree oil is highly concentrated and must be diluted before application:
Mix 1-2 drops with a tablespoon of a carrier oil (such as coconut or jojoba oil) or water.
Never apply pure essential oil directly to the skin, as it can cause irritation.
By using tea tree oil correctly, its natural properties can effectively aid in managing acne and improving skin health.
4.3- AZELAIC ACID:
Azelaic acid is a dicarboxylic compound derived from natural sources such as grains (wheat, barley, and rye). It is widely used in dermatology due to its antimicrobial, anti-inflammatory, and keratolytic properties, making it an effective treatment for skin conditions like acne and rosacea
MECHANISM OF ACTION
- Antimicrobial Action: Inhibits the growth of bacteria such as Cutibacterium acnes (associated with acne) and Staphylococcus epidermidis, both of which contribute to inflammation and lesion formation.
- Anti-Keratolytic Effect (Regulation of Keratinization): Normalizes the keratinization process within hair follicles, preventing the buildup of dead cells that can clog pores and form comedones.
- Anti-inflammatory Properties: Reduces the production of reactive oxygen species (ROS) and blocks the activity of pro-inflammatory cytokines, decreasing redness and inflammation.
- Tyrosinase Inhibition: Interferes with tyrosinase activity, a key enzyme in melanin production. This makes azelaic acid effective in treating post-inflammatory hyperpigmentation (PIH), a common condition in individuals with acne.
- Sebum Regulation: Although it does not directly reduce sebum production, it improves skin texture by minimizing pore blockages.
Typically available in 15%-20% concentrations in creams or gels.
Requires consistent use for 4-8 weeks to see results.
4.4. ISOTRETINOIN
Isotretinoin is an oral retinoid derived from vitamin A, primarily used to treat severe, nodulocystic acne resistant to other treatments. It is one of the most effective medications available for acne as it addresses the main causes of this condition.

Isotretinoin Addresses Acne Through Multiple Mechanisms, Making It Highly Effective:
- Reduction of Sebum Production: Isotretinoin reduces the size and activity of sebaceous glands, significantly decreasing sebum secretion.
This eliminates the environment conducive to the growth of Cutibacterium acnes.
- Anti-inflammatory Effect: It reduces the production of pro-inflammatory cytokines, decreasing inflammation associated with acne.
- Inhibition of Keratinization: It normalizes the renewal of skin cells within the hair follicle, preventing the formation of comedones (clogged pores).
- Indirect Antibacterial Action: By reducing sebum and normalizing the follicles, it creates an unfavorable environment for Cutibacterium acnes, lowering its population.
DOSAGE:
- Standard Dose: Between 0.5-1 mg/kg of body weight per day.
- Cumulative Dose: The total treatment typically reaches 120-150 mg/kg to reduce the likelihood of relapse.
- Low Dose: Used in some cases to minimize side effects, though it may require a longer treatment duration. Frequently, very low doses over prolonged periods are effective with minimal or no side effects.
4.5-KETOCONAZOLE
What is Ketoconazole?
Ketoconazole is a broad-spectrum antifungal medication belonging to the imidazole family. It is primarily used to treat fungal infections but also has antiandrogenic and anti-inflammatory properties, making it useful for certain skin conditions, including acne.
Mechanism of Action of Ketoconazole
- Antifungal Effects: Inhibits the synthesis of ergosterol, a key component of fungal cell membranes, eliminating or preventing their growth.
It is effective in treating skin infections caused by fungi, such as Malassezia, a yeast associated with seborrheic dermatitis and fungal folliculitis, which may coexist with acne.
- Antiandrogenic Effect: Blocks the conversion of testosterone to dihydrotestosterone (DHT) by inhibiting the enzyme 5-alpha reductase.
This reduces hormonal stimulation of sebaceous glands, decreasing sebum production, which is a key factor in acne development.
- Anti-inflammatory Properties: Reduces skin inflammation by inhibiting the synthesis of pro-inflammatory mediators.
- Antimicrobial Effect: While its primary action is against fungi, it also limits the growth of bacteria such as Cutibacterium acnes, which contribute to inflammatory acne.
KETOCONAZOLE AND ACNE
Seborrheic Acne: Acne may be related to excessive sebum production and the presence of Malassezia. By controlling these factors, ketoconazole can significantly improve lesions.
Fungal Folliculitis:
Often mistaken for acne, this condition involves the infection of hair follicles by fungi. Ketoconazole is highly effective in these cases.
Sebum Regulation:
In patients with acne associated with oily skin, ketoconazole can help regulate sebum production.
Hormonal Acne:
Although not a first-line treatment, its topical antiandrogenic effect can benefit women with mild to moderate hormonal acne.
Forms of Use for Ketoconazole in Acne
As a Shampoo:
Apply to the affected skin, leave on for 3-5 minutes, and rinse thoroughly.
As a Cream:
Apply a thin layer to the affected areas once or twice daily.
5. CONCLUSION
Steroid-induced acne is a common issue that can be avoided, treated, and resolved with proper attention. If neglected, it can leave severe scarring, damaging physical appearance and confidence.
The causes are clear: androgen and estrogen imbalances, altered lipid profiles, and inflammation. Proper hygiene in androgen-sensitive areas (back, neck, chest) is essential.
For mild acne, start with gentle treatments like benzoyl peroxide and tea tree oil. For more severe cases, isotretinoin is often the best option, with professional guidance.


